Last Tuesday, 27-year-old co-pilot Andreas Lubitz deliberately crashed a Germanwings Airbus A320 jetliner into a mountainside in the French Alps, killing 150 people. The plane’s captain, Patrick Sondenheimer, had stepped out of the cockpit, during which time Lubitz locked the door and began the aircraft’s lethal descent. Sondenheimer reportedly tried to regain access to the cockpit using an axe, while Lubitz showed no emotion and spoke no words during the final moments of his life. On the black box recording that also captured the terrified screams of passengers, Lubick can be heard breathing normally.
Theories of Lubitz’s motives proliferated in the aftermath of the crash. Though Lubitz left no manifesto and made no statement at any time as to the meaning of his actions, some are still convinced his was an act of terrorism. An ex-girlfriend of Lubitz’s has come forward to claim that the co-pilot fantasized about fame and notoriety, and must have become distraught when he realized his dreams of a job at Lufthansa, the largest airline in Europe, were unlikely to come true. Author Mark Ames, who has written a book on rage killings in the United States, has raised the possibility that Lubitz’s actions were those of a disgruntled employee, not unlike the postal shootings of the '80s and '90s.
It’s possible that all of these elements factored into Lubitz’s ultimately baffling decision to kill himself and over one hundred innocent people. But underneath each of these themes runs another current, which continues to gain strength as the investigation wears on: Lubitz’s struggle with depression.
According to friends of the man, he suffered from a depressive episode of burnout in 2009, and was forced to withdraw from pilot training as a result. Investigators searching Lubitz’s home found several doctors’ notes attesting that he was too ill to work, including one from the day of the crash; evidently none of these notes, one of which was torn up, had been delivered to Lubitz’s employer. Medications for “severe depression” were also discovered in Lubitz’s residence. And on Monday, according to the New York Times, the German prosecutor in Düsseldorf said that Lubitz had been treated for “suicidal tendencies” before he got his pilot’s license.
There is little doubt that Lubitz was suffering intensely from depression at the time of his death, which may be of little meaning to those devastated by the monstrous enormity of his final act. But Lubitz's case raises an important question: Who are the people usually harmed by depression and is there any hope for intervention in cases of seemingly sudden and inexplicable suicide?
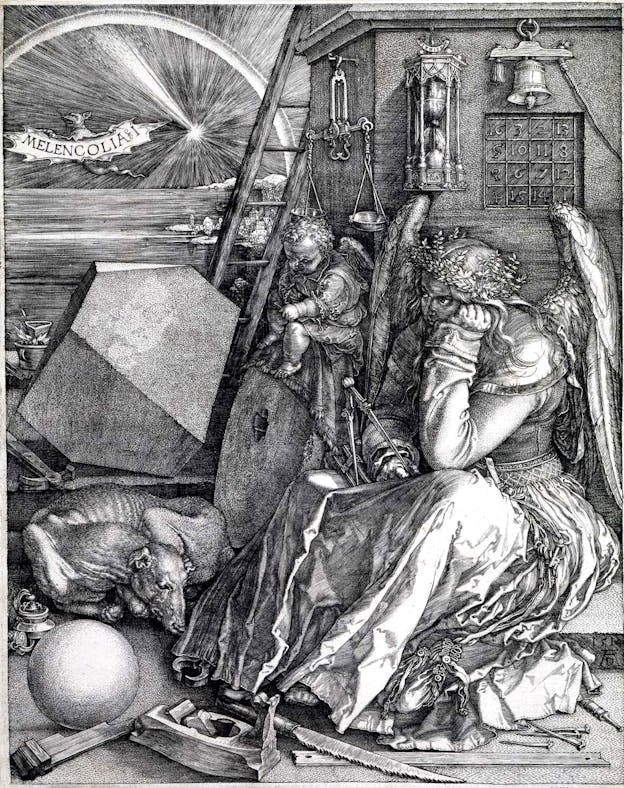
In 2011, Danish filmmaker Lars von Trier released Melancholia, starring Kirsten Dunst as Justine, a deeply depressed woman seemingly unmoved even as a rogue planet slings into collision with earth, destroying all life. The film received mixed reviews, but even its most incisive critics, such as The New Yorker’s Richard Brody, lauded its depiction of depression: “[T]he one true thing in Melancholia,” Brody wrote in his review, “is the depiction of Justine’s depression, with her utter passivity and the blank look in her eyes.” Some 500 years prior to von Trier’s film, German artist Albrecht Dürer created an engraving entitled Melancholia I. Its scene seems a forbearer to von Trier’s film, with an impassive figure seated motionless, surrounded by unused instruments and a rapidly depleting hourglass as a celestial disaster unfolds in the background. Time is running out, in other words, and the engraving’s subject is too troubled to care.
In identifying cognitive turmoil with depression, Dürer and von Trier hit upon one of the chief signs of the illness. “One of the cardinal symptoms of Major Depressive Disorder … is impairment in concentration,” Dr. Anthony Charuvastra, a voluntary clinical assistant professor in the Department of Child and Adolescent Psychiatry at NYU Langone Medical Center, told me. “People suffering MDD often describe this as slowed thinking, indecisiveness, or trouble organizing thoughts.” Unlike sadness or sorrow, depression exerts a kind of downward pressure on the mind, producing, in its most severe instances, impairments in thought and judgment, which can manifest itself in a variety of ways. A 2013 study of patients with HIV and depression found, for example, that “depression … threatens an individual’s ability to enact effective coping responses,” and that “ineffective coping, in turn, puts a person at risk for missing single doses of medication or having extended treatment interruptions.” Depression interferes with treatment compliance in other illnesses, too.
Which is to say, taking care of yourself when depressed is not as simple as it sounds, even when all medical options are available. In Lubitz’s case, every piece of the German healthcare system worked: He had access to treatment and medication, and his doctors had identified his illness and that he should not be working, and had given him the resources to make as much known to his employer. It was Lubitz himself who failed to make use of the options at his disposal, either out of concern for his employment—not an altogether rational consideration, given the alternative —or simply because depression, with all its attendant anxieties about worthlessness, failure, and futility, made pursuing healthy choices seem pointless or impossible.
“Depression, for me, is marked by lacking the energy needed to do any of the things that make life worth living,” said Clark, whose surname is omitted for privacy (as are the surnames of other sufferers of depression I interviewed), a 23-year-old non-profit consultant from Virginia. In an interview, he recalled that “at its worst times, I feel constantly fatigued and can only wish that something outside of me will end my life already.” Andrew, a 21-year-old Manhattanite who works in radio, put it this way: “You get trapped in your own head, sparring against yourself until suicide doesn’t seem like a way out, it seems like the only rational thing you can do.”
Despite these effects, the victims of the vicissitudes of depression are vastly its own sufferers. People tend to largely overestimate the amount of violent crime committed by people with mental illnesses and underestimate the rate at which mentally ill people are victimized themselves. Lubitz’s mass-murder-suicide is an extraordinary exception among depressed people, and it is worth emphasizing that depressed people represent no special risk to others. But each suicide is its own loss, whether or not others are harmed in the process. So how can we know who is at risk, and who is not?
A prevailing theory of suicide holds that the decision is usually impulsive and sudden. “In people with severe depression who are suicidal, the thing we worry the most about is impulsivity,” Dr. Charuvastra said. “Many studies of suicide, at both the individual level and population level, demonstrate that impulsivity is one of the major risk factors that can catalyze suicidal thoughts into action.”
There is good reason to accept this narrative. Suicide prevention measures, like reducing the number of pills in blister packs or bottles to non-lethal amounts, have proven effective at bumping down the number of pill-induced suicides, suggesting that small complications can put people off of abrupt intentions. People who survive suicide attempts—say, by leaping off the Golden Gate Bridge—often report that they regretted the decision to attempt suicide before realizing their plans had gone awry. Survivors also often link their suicide attempts to moments of severe crisis, furthering the hypothesis that much self-destruction is a product of despair and impulse rather than premeditation.
In Lubitz’s case, this is both comforting and disconcerting. On one hand, it might come as a cold comfort to know that there was possibly no terroristic intent in the co-pilot’s decision to end his life and steal the lives of 149 others after all, and that he may well have made his decision to do so in mere moments. Yet, on the other hand, the idea that severe depression can produce sudden, unexpected acts of impulsive destruction makes the problem seem intractable. If suicide is, on some level, like a lightning strike in the mind, how can we prevent it and protect ourselves from those who might be at risk?
Professor Michael Anestis, director of the Suicide and Emotional Dysregulation Lab at the University of Southern Mississippi, thinks there is more to suicide than the impulse theory.
“Where everybody would agree on impulsivity is that impulsive folks attempt and die by suicide more than non-impulsive folks,” Dr. Anestis told me. "Where I disagree with most is that it stops at that level.” Contrary to the idea that suicide is born of an instantaneous burst of emotional pain, Dr. Anestis believes that the capability to commit suicide develops over long periods of time, during which a person becomes habituated to both the pain and the idea of dying.
Working with army personnel, Dr. Anestis and his colleagues have found that those who have completed basic training, for example, have a higher suicide capability than those who have not, suggesting that learning to cope with the idea of death and significant physical stress builds up the endurance it takes to go through with suicide. Thus, there may be more time between a person’s initial consideration of suicide and the act itself than impulse theory would allow—and more of an opportunity for intervention than many suspect.
Still, Dr. Anestis notes that “we’re not particularly good at detecting risk, who’s going to do it and when.” There are very good reasons people suffering from severe depression may not reveal it to others, including professional and personal risks. Sean, a 25-year-old Canadian law student, told me, “As for friends and colleagues, I would never want to [talk about mental illness]. Law school, especially the one I go to, is a very competitive environment… You are always competing directly with one another, essentially. Concurrently, I am in my final year, yet I do not have a job lined up yet… This makes me very reluctant to bring up anything of the sort to anyone.” John, a 35-year-old music teacher from Texas, felt the same. “Often I wish I could take back having told my general friend population about it,” he told me. “I find that if managers or co-workers find out about my depression, they are far less likely to consider me reliable, trustworthy, capable, or worthy of leadership roles.”
For this reason, Dr. Anestis feels that reversing stigma surrounding mental illness is a vital step in reducing suicides. “The best treatments for suicidal behaviors aren’t to isolate [people with suicidal thoughts], take them out of employment, and make them feel less connected to others,” he says. “So in an ideal world, you would make available an opportunity to get treatment without impacting your work status. Nobody has shown me evidence that says people experiencing [suicidal] ideation are less capable of doing their jobs.” Dr. Anestis emphasized that out-patient therapies, which can remain unknown to employers, are very effective at treating suicidal depression.
Preventing suicide requires a web of support: adequate and accessible mental healthcare, employment provisions that protect employees struggling with mental health problems, and, perhaps least often acknowledged, a society that is willing to express honest concern for people in pain.
One study found that simple follow-up postcards sent to patients admitted to hospitals for self-poisoning helped reduce readmissions. Dr. Anestis isn’t surprised by the finding: “We’re social creatures,” he says. “We’re looking for any way to connect.” Reaching out to people suffering from depression and including them in the life of society, from family, to friendship, to employment, might be one of the most significant tools we have in preventing tragic loss.
In cases like Lubitz’s, it is hard to strike a proper balance between holding a person responsible for what they have done and taking into account factors, like severe depression, that may have mitigated their judgment. So it is worth being clear: Lubitz is guilty of his crime, and the realities of depression and suicidality are worth considering, not to tidy up his reputation, but to help establish a safer, more conscientious world for those left behind. It is the best we can do.
